Uncovering the History of Obesity/Belly Fat!
The history of obesity and belly fat is funny how our understanding and perception of it has evolved.
Back in ancient times, belly fat was seen as a symbol of wealth and health. Nowadays, it is unhealthy and unattractive. In this article we will take a look at the history of obesity, the science behind it, plus much more.
Back in the day obesity was a positive thing similar to a big bank account
today.- Adolphe Quetelet’s BMI revolutionized population health assessments, but individual well-being requires considering clinical evaluation and other markers as well.
Obesity is caused by genetics, environmental and microbiome factors combined with an excessive availability of food and decreased physical activity. Strategies for losing fat include diet, physical activity & medications/supplements.
The Evolution of the Perception of Obesity

Throughout human history, obesity has been perceived in many different ways. In ancient times, having a lot of body weight was viewed as a symbol of wealth and health. Obesity was rarely observed back in the day, and those who were overweight were typically seen as prosperous and productive.
Since then, medical knowledge has come a long way, and the perception of obesity has shifted dramatically. Nowadays, obesity is seen as ugly and known to have many health risks.
Obesity in Ancient Times
In the days of hunters and gatherers, food intake was very inconsistent. The ability to store fat was seen as a huge advantage.
If you were in a situation where you couldn’t eat in weeks, a fat man could survive while a skinny man wouldn’t. The average man didn’t have the luxury to gain weight because food was very scarce. That’s why there was a different view on obesity in early human history.
Back in the Stone Age, Europe had some stylish “thick” figurines. These mysterious nude ladies from over 20,000 years ago were actually considered the cream of the crop of sexy women. Back then, extra body weight was seen as a positive thing.
In 1930, Newburgh and Johnston said that obesity was an energy surplus. This is the seed that formed our current understanding of the link between food consumption and weight gain.
The 19th Century and Changing Attitudes
In the 19th century, medical professionals started to view obesity as a health risk and the cause of chronic diseases. This was shocking to some because people used to believe that carrying excess weight was healthy. In1905 William Osler wrote a book and said that obesity was caused by overeating. He was implying that excessive caloric intake played a huge role in excess body fat.
This changed how we viewed obesity and laid the foundation for our current understanding of its health consequences.
The 18th-centurys view of obesity as a sign of wealth and safety was now gone. By the 19th century the World Health Organization linked obesity to fatigue, gout, and breathing difficulties.
The Creation of Body Mass Index (BMI)
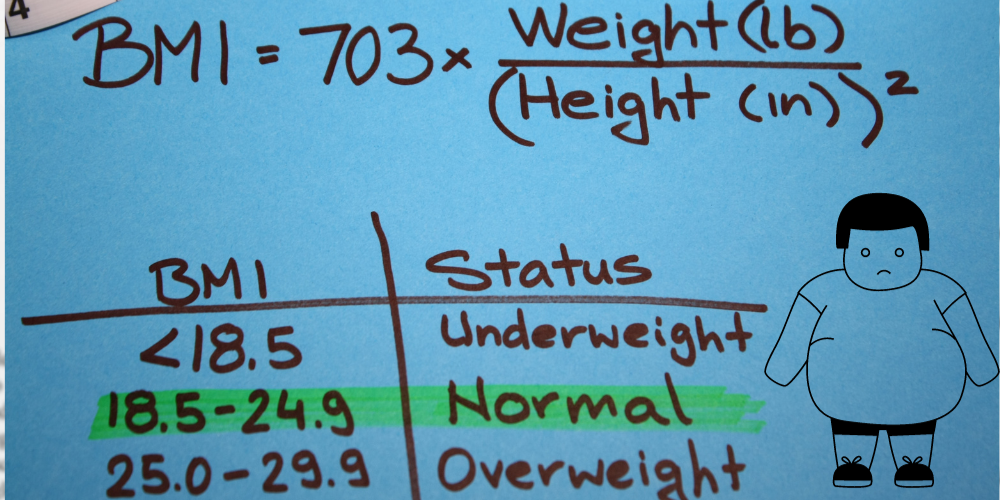
The Body Mass Index came out in the mid-19th century as a way to measure obesity and the populations health. It was created by Adolphe Quetelet, BMI is a measure of body fat based on a person’s height and weight.
Most people with a BMI in the range that is considered obese usually have a high amount of body fat. BMI has faced a lot of criticism because it can be inaccurate when measuring an individual’s health and body composition.
Since BMI is only based off height and weight it can give a false result. For example, if a man is 5ft 200lbs he will be considered obese, even if he is all muscle.
Adolphe Quetelet’s Contribution
Adolphe Quetelet’s development of the BMI formula was made to evaluate population health. It provided an essential tool for understanding the prevalence of obesity and its potential health consequences. The importance of Quetelet’s contribution to obesity research cannot be overstated! It allowed for large-scale assessments of body weight and health on a population level.
Nonetheless, it’s noteworthy that BMI isn’t the only parameter that determines an individual’s overall health and development. Clinical evaluation and other markers must be taken into account to provide a comprehensive understanding of a person’s well-being. High BMI in children has been associated with an increased risk of future health complications and the potential development of disease.
Limitations and Criticisms
Despite its widespread use, BMI has faced numerous criticisms for its lack of accuracy in assessing individual health and body composition. One such criticism is that it does not accurately account for muscle mass! This can result in individuals with a high muscle-to-fat ratio being classified as overweight or obese.
Additionally, BMI does not take into account the distribution of body fat. This can be a crucial factor in determining health risks. For example, individuals with a high waist circumference, indicative of abdominal obesity, may have an increased risk of health issues even if their BMI falls within a lower range. This has led to the recommendation of waist circumference measurements in obese adults to provide a better assessment of health risks.
Nutrition Science and Obesity
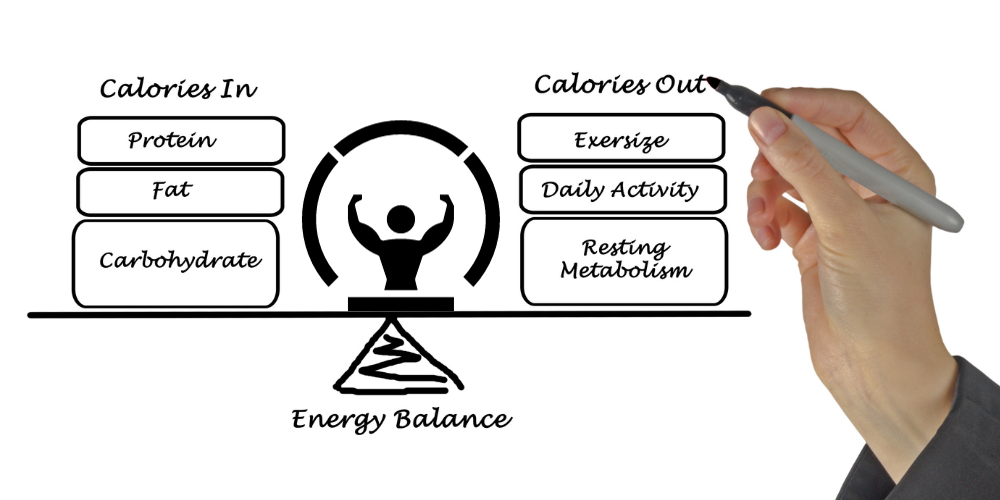
Advances in nutrition science have provided us with a better understanding of the correlation between food, energy balance, and obesity. The thermodynamics of food utilization by the body, the metabolism of nutritional elements and the refined definition of obesity have all had a huge impact on improving our knowledge and management of obesity. This has been a major breakthrough in the associated research field!
For example, Mayer’s 1953 observation that obese mice were less active suggested that the “calories out” factor played a role in obesity.
Thermodynamics and Food Utilization
The study of thermodynamics has provided amazing insights into how the body uses and stores energy from food. Research on the thermodynamics of food metabolism has demonstrated that excessive subcutaneous and visceral fat accumulation results from an imbalance between the energy ingested through food and the energy expended through daily activities.
In 2015 a metabolic balance study revealed that a 30% caloric restriction with stable protein and decreased carbohydrates led to increased fat oxidation! It also decreased carbohydrate oxidation and no real change in body fat. However, decreasing the fat content of the diet resulted in a decrease in body fat.
This research shed light on the complex relationship between food intake, energy expenditure, and body fat accumulation.
The Role of Macronutrients
Research on macronutrients has provided us insights into how many different nutrients may be linked to obesity. Studies of gastrointestinal absorption, the feeling of satiety, and nutritional-deficiency disorders have contributed to our understanding of the relationship between macronutrients and obesity.
One key finding in macronutrient research is the role of ghrelin, an orexigenic hormone involved in meal initiation. Ghrelin levels have been found to be elevated in patients with Prader-Willi syndrome and low in patients with simple obesity. This showed the complex relationship between macronutrients and obesity.
Research on macronutrients has expanded our understanding of the role of many nutrients linking to obesity. This knowledge can help dietitians and regular people create a strategy to fight the growing obesity epidemic.
Factors Contributing to the Rise in Obesity

Obesity is a complicated issue that can be caused by genetics, environment, and the gut microbiome. The energy storage hypothesis of obesity suggests that genetic and hormonal factors play a role, involving organs such as:
the brain
adrenal gland
pancreas
adipocyte
However, these factors alone cannot explain the current worldwide epidemic of obesity. I believe it is due to an excessive availability of food combined with decreased physical activity.
Genetic Influences
While genetic factors can definitely play a role in obesity, they do not fully explain the obesity epidemic. There are rare cases of obesity can be caused to changes in a single gene, like MC4R. Genetic and epigenetic variations can influence metabolic pathways and neural regulation.
Obesity has a heritability range of 40-70%, as reported by Stunkard et al. The FTO gene has emerged as the leading genetic factor linked to obesity.
However, genetics alone cannot account for the rapid rise in obesity rates. While genetics can make people more prone to being overweight, other factors such as lifestyle, exercise, and diet are important.
Environmental Factors
Lifestyles and environments play a huge role in the rise of obesity rates. Factors like restricted access to nutritious foods and limited availability for physical activity opportunities are a big part of obesity.
Changes like reduced physical activity, poor diets, excessive screen time, all contribute to the rising rates of obesity.
This is even more true for children nowadays. Factors like parent feeding practices, limited access to parks, sidewalks, and public transportation contribute to obesity in the population.
Recognizing and addressing these environmental factors is key in tackling the obesity epidemic.
The Role of the Gut Microbiome
The gut microbiome has been implicated in the development of obesity, but the relationship is complex. Most people don’t even know what it is. The gut microbiota plays a crucial role in adiposity, metabolism, and gastrointestinal functions. Changes its composition have been connected to the rise of obesity.
However, the link between the gut microbiome and obesity is complex and still not completely understood. Further research is needed to fully understand the complex relationship between the gut microbiome and obesity. Hopefully potentially paving the way for new prevention and treatment strategies.
Health Consequences of Obesity
Obesity is associated with numerous health risks, including:
High blood pressure
High cholesterol
Type 2 diabetes and its complications
Coronary heart disease
Stroke
Gallbladder disease
Osteoarthritis
Sleep apnea
Respiratory problems
Endometrial, breast, prostate, and colon cancers.
These health risks are real and should be taken seriously to help manage and overcome severe obesity.
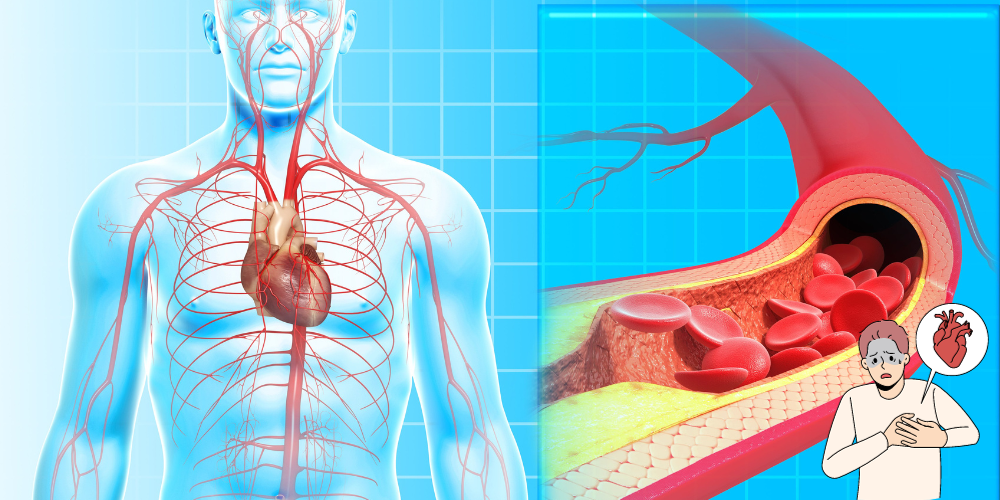
Cardiovascular Disease
Obesity is a major cause of cardiovascular disease, significantly increasing the likelihood of developing cardiovascular risk factors such as:
dyslipidemia
type 2 diabetes
hypertension
insulin resistance
Abdominal obesity, belly fat in particular, has been a significant risk factor for cardiovascular disease on a global scale.
Individuals who are obese face a higher likelihood of experiencing cardiovascular-related fatalities. Cardiovascular disease ranks as the leading cause of death among those that are obesity. Tackling obesity through lifestyle changes and medical treatments is key to reducing the risk of cardiovascular disease.
Diabetes Mellitus
Obesity is the biggest risk factor for type 2 diabetes, as it is linked to insulin resistance. This also causes a decrease in the sensitivity of the body’s cells to insulin, leading to higher blood glucose levels. The accumulation of body fat has a huge effect on the functioning of the pancreas. That is responsible for controlling blood glucose levels.
Controlling obesity is key in both the prevention and management of diabetes mellitus. Weight loss has been known to enhance insulin sensitivity and stop the risk for disease.
Chronic Kidney Disease
Obesity has been linked to kidney disease, both directly and indirectly through its association with diabetes and hypertension. Chronic Kidney Disease (CKD) is a long-term condition. CKD is basically impaired kidney function, leading to the inability to filter waste and toxins from the body.
Obesity-related glomerulopathy is a specific kidney disease associated with obesity. Recent research has showed a direct link between obesity and chronic kidney disease and its outcomes. Tackling obesity can help in minimizing the risk of developing CKD and its associated complications.
Strategies for Combating Obesity

To address obesity, a multifaceted approach is necessary, involving a good diet, physical activity, and medical interventions when needed.
Strategies for combating obesity include:
Implementing early care and education policies
Promoting family healthy weight programs
Enhancing physical activity
Decreasing energy intake
Encouraging a healthy weight trajectory for children.
Dietary Interventions
Reducing calorie intake and improving diet quality are key factors in preventing and treating obesity. Dietary interventions can include:
Energy restriction through weight loss diets
Controlling portion size
Reducing intake of carbohydrates, total fat, and saturated fat
Increasing intake of proteins and fiber
Nutrition education
Limiting foods and beverages high in added sugars, saturated fat, and salt
Promoting access to nutritious food choices and encouraging healthy eating habits are key when addressing obesity at a population level.
Physical Activity
Regular physical activity is essential for maintaining a healthy weight and preventing obesity-related health issues. Physical activity offers numerous benefits, including:
Enhanced cardiovascular health
Augmented muscle strength and stamina
Increased flexibility
Improved mental health
Augmented energy levels
A combination of aerobic exercises, such as running, swimming, and cycling, and strenth training, such as weightlifting, can help maintain a healthy weight and reduce the risk of developing obesity-related health conditions.
Medical Interventions
In some cases, medications or surgical interventions may be necessary to treat obesity and its complications. Medications such as leptin therapy and GLP-1 can facilitate weight loss and reduce appetite and reward. Surgical interventions, such as gastric balloon or surgery, may be utilized to decrease stomach volume or the length of the intestines.
Bariatric surgery, in particular, has been shown to result in both weight loss and control of type 2 diabetes, as it impacts gut hormone secretion, including peptide YY (PPY) and glucagon-like peptide 1 (GLP-1).
While medical interventions can prove effective in tackling obesity, they should be seen as part of a broader approach incorporating lifestyle modifications and preventative measures to combat obesity. This is a last resort!
Summary
The history of obesity is a complex narrative that evolves as we learn more about its causes and consequences. From ancient times to present, our understanding has shifted, recognizing its health risks and developing strategies to address and prevent it. By embracing a multifaceted approach, we can combat the global obesity epidemic and promote healthier lifestyles for all.
Frequently Asked Questions
What is the history of obesity?
Obesity has a long history, with origins stretching back at least 25 000 years. The eighteenth century, its impact on quality of life began to be recorded. In the nineteenth century it was recognized as a cause of ill health. In the twentieth century, morbid complications and increased mortality associated with obesity became obvious.
Were people overweight in 1800s?
In the 1800s, being overweight was not seen as a health problem since most people were usually thin due to their labor-intensive lifestyle. Also, according to Victorian medicine, individuals who were overweight and healthy were categorized as ‘plump’. There were overweight people in the 1800s just not as many as there are today.
What are the main criticisms of BMI as a measure of obesity?
BMI has been heavily criticized for not taking into account individual body composition and muscle mass.
How do genetic factors contribute to obesity?
Genetic variants can increase an individual’s susceptibility to obesity, as evidenced by rare cases of single gene-influenced obesity, and epigenetic variations may also alter metabolism and neural regulation. Ultimately, genetic factors can contribute to the obesity epidemic.
What are some environmental factors have been linked to the increase in obesity rates?
Today’s lifestyle and environmental factors, like not having enough healthy food options, less chances for physical activity, and even lack of street lighting, have been connected to a rise in obesity rates.